Hey there, welcome to Part 3 of this Getting Ready for Residency Series where I’ll give tips on how to do amazing as a pharmacy resident on rotations and throughout the residency year! If you haven’t already, check out Part I about what to do before starting residency, and Part II about what to do during orientation month to help set you up well. Part IV will be about staying organized during residency and should be out by August if everything goes to plan!
Starting rotations can be intimidating as a newly minted resident and an *actual* licensed pharmacist. From my experience, each rotation was very different and each preceptor’s style was different as well. In all transparency, during residency, your clinical rotations are a small portion of all of the things you’ll be doing in residency. In addition to your clinical rotations, you’ll have meetings, admin work, staffing, teaching/precepting responsibilities, committees…etc. Looking back, I believe what helped me the most in terms of my rotations was the pre-work/forethought before starting a rotation, staying organized throughout the year, and being transparent with my preceptors about things I wanted to learn/topics I wanted to better understand (which came with time) based on my goals. I’ll be sure to thread all the things I did and the resources I used below. So let’s jump right in with pre-rotation preparation!
PRE-RESIDENCY ROTATION PREP TIPS:
1. Read the rotation syllabus and then read it again!
The syllabus for your rotation is likely located on Pharmacademic and/or on some sort of shared drive/folder. If you aren’t sent the syllabus ahead of time, you should definitely ask during the pre-rotation meeting invite to your preceptor (which I talk about below). When reading through the syllabus, pay attention to any special requirements, dates, presentations/projects, required prereading (if any), topics that the rotation will cover, and the preferred communication of your preceptor. Jot down any questions you have about the syllabus and if there is anything you want to clear up during the pre-rotation meeting.
2. If your co-residents had that rotation before you, ask them for tips!
As I spoke about in Part II, your co-residents will be so helpful and needed during your residency year. If you’re going on a new rotation, ask your co-residents (PGY-1s and PGY-2s) who had the rotation if they have any tips. It’s so nice to get some inside scoop on how to handle the rotation and things to expect as well as any unspoken “rules” of the rotation. Don’t be shy!
3. Meet with your preceptor
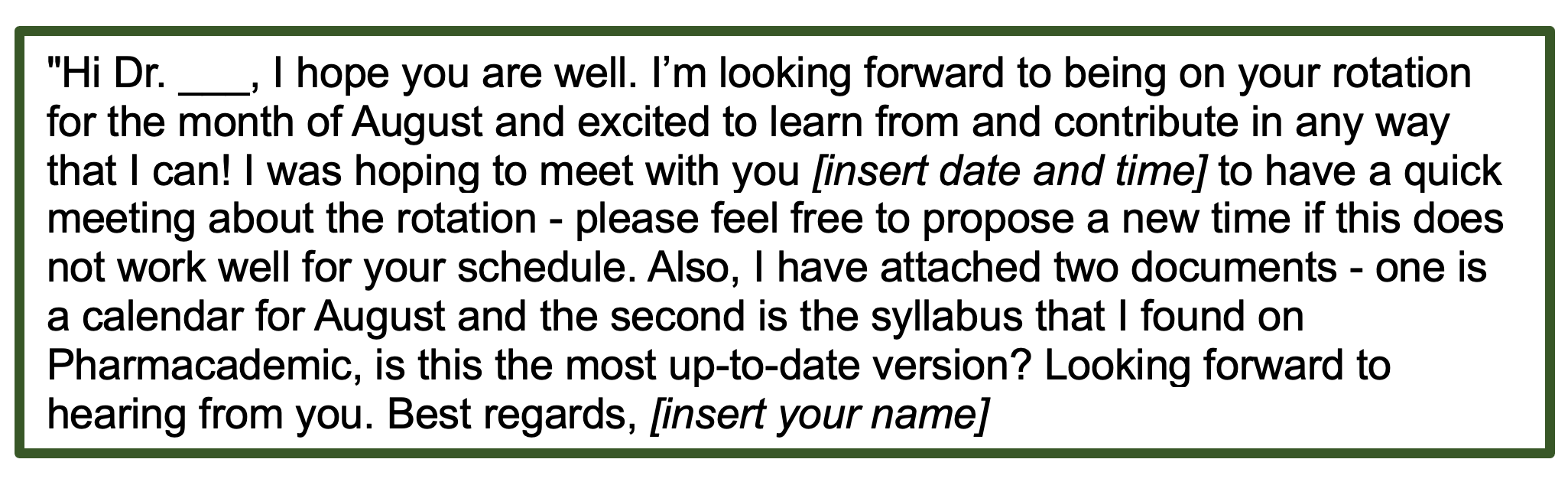
When I was a student, the general rule of thumb was to contact your preceptor about 4 weeks before starting. However, in residency, it’s generally a shorter amount of time since everyone is at the same hospital. Personally, I contacted them ~2 weeks before my rotation. When I had an off-site rotation, I contacted those preceptors ~4 weeks before the rotation – ultimately, follow your program’s guidance as each program differs. When contacting my soon-to-be preceptor, I would use the Outlook Calendar feature to determine when they’d be free and schedule a pre-rotation meeting. In the meeting invite, I’d do a short introduction, ask if that date/time was good for them, and I’d attach two documents – one would be the syllabus that I found and I’d ask (in the email) if it was the most recent one & the second attachment would be a draft calendar for the rotation month (more on this later). For the meeting, we’d meet for ~30 minutes but keep in mind some preceptors would rather not meet ahead of time but prefer to do a mini run-down on the 1st day of the rotation, so it depends.
Not sure what to say in the email? I got you! See below
What to prep for your meeting: Overall, bring a positive and excited attitude! Bring a physical copy of the syllabus and calendar. If you know your career goals and/or what you want to learn on rotation (including strengthening your weaknesses) be vocal about it. One example could be – let’s say you’re weak in infectious diseases and going on an ICU rotation, you can vocalize that so that your preceptor can look out for opportunities for you to improve. The same goes for your career goals – if you’re going into an ICU rotation but you are interested in oncology, they will look for opportunities for you to learn oncology in the ICU. Additionally, review the calendar you sent with your preceptor, review any dates that you won’t be able to attend because of conflicts/meetings/training, and highlight any other responsibilities such as if you’ll be on code blue coverage, a coinciding longitudinal rotation…etc). Also, use that time to ask any questions about the syllabus, how rounds are structured, if there are any preparation readings they recommend, their expectations…etc. Really listen to them when they talk and understand what makes for a successful rotation. Lastly, if it is not plainly spelled out in the syllabus, ask when you’ll need to have projects for that rotation completed (such as topic discussions, and presentations) so that you can put it in your calendar and plan ahead.
All about the calendar: Above, I talked about attaching a calendar & bringing it to the first meeting. Having a calendar for each rotation really allowed me to plan ahead & have my preceptor and I be on the same page about deadlines, evaluations, meetings…etc. Personally, what I would do is create a calendar on Microsoft Word (example below) and email it to them prior to our pre-rotation meeting and bring it to the meeting. It was a bare-bones calendar that would include what other meetings/commitments/due dates I had that month as well as proposed dates for topic discussions and presentations/journal clubs etc. Additionally, in my program, for every rotation, we had a project/WFH day so I would propose the dates of that as well to my preceptor. We would review the bare bones calendar during the meeting, and then based on the discussion, move things around and definitively schedule when my presentations/projects would be and add in any other meetings they needed me to attend. By the time the rotation started, I would email and hand them a clean & final copy (example in the photo below). It is important to be flexible though because many things can change during the rotation month. Here is just an example of what a calendar may look like (part IV of this series about organization will have more on how calendars saved me time and time again in residency).
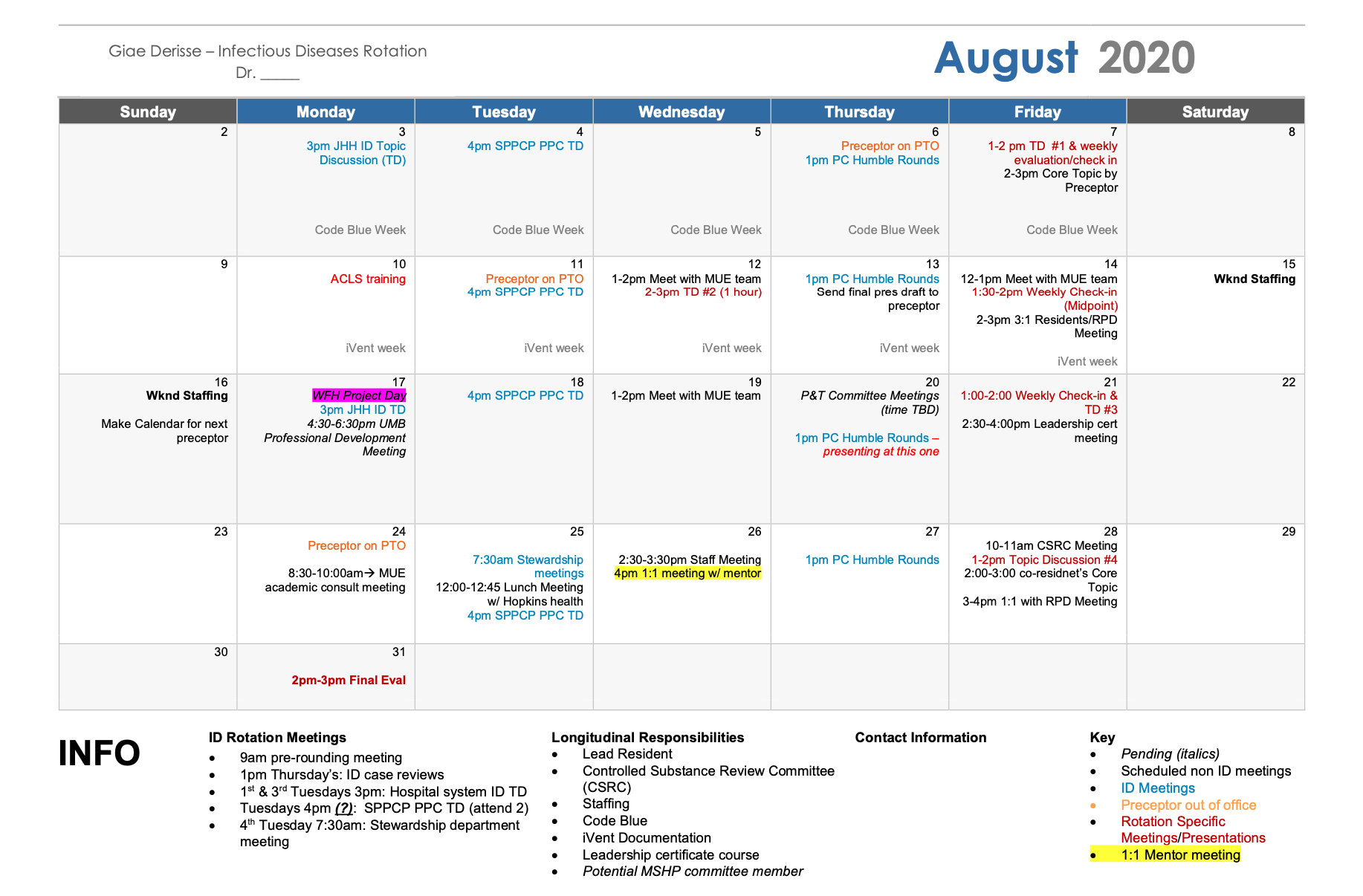
This is a rough example of the final calendar I would have at the start of the rotation. As you can see, it has all the meetings I had for the month (rotation-based meetings as well as meetings outside of my rotation) with the times. It also shows different commitments I have outside of the rotation such as being on code blue duty the 1st week, having to do the documentation for the department the second week, being lead resident…etc so that the preceptor has a general awareness of what is going on. This helped to create transparency around the rotation and clear expectations early on (I did this calendar for basically all my rotations).

click the images to go directly to the original posts!
WHAT TO DO WHEN YOU’RE ON THE ROTATION:
Now that you’ve done all the pre-rotation work – what’s next? Starting your rotation! Being an *actual* pharmacist after being a student for many years can feel intimidating, I get it! With lots of time, taking initiative, asking questions, and reading you’ll start to get the hang of things. Even entering into clinical pharmacy post-residency, there will still be A LOT to learn so don’t put so much pressure on yourself that you need to know everything (even your preceptors are continuously learning). Keep reading for some quick bullet points on things I wish I knew going into it!
- Introduce yourself to the team that you’ll be working with during the rotation and build rapport with them throughout. During my residency, the medical and PA residents were also rotating, so it was hard to keep up, but please do put in the effort, it’ll go a long way. Getting to know the role of each member of the team and the general flow is important. This was a little difficult for me because I’m a little introverted and observant before jumping in, so it took time, but I soon realized how fast time flies since the rotations are only 5 weeks.
- Pre-round on your patients. Every program is different in its expectation of residents and the expectations do change as the year progresses, but I would say start with a small number (1-3) of patients that are recent admits to workup and asses for recommendations & during the time with your preceptor, be sure to ask questions/discuss. As the rotation and year progresses, challenge yourself to take on more & be vocal if you’re having a hard time keeping up. Remember it’s important to learn how to walk before you can run!
- Take initiative! If there’s a pharmacotherapy-related question that comes up during rounds, offer to look it up/look into it – don’t just shy away in the background.
- If you don’t know something be honest about it. Don’t make up an answer, rather consider saying something to the effect of: “Hmm that’s a good question, I’m not 100% sure about that, let me look into it and I’ll get back to you ASAP.”
- Become familiar with the nurses as well. Even though they may have varied shifts, they usually appreciate knowing who the pharmacists on the floor are and aren’t shy about asking questions about the status of medication delivery, interactions, administration instructions, etc. Those questions will not only help you learn more about meds but also about the operational side of pharmacy which is just soo important.
- Next, look for small wins often and take on responsibilities to learn. This can look like reviewing the medications the patient is on in the hospital – are the doses correct for the indication? Is the route of admin right (if they have a feeding tube, it shouldn’t say p.o.), look to see which meds a patient takes at home and if they aren’t getting it inpatient, but should look into it [for example, (1) if a patient has hypertension and is on three medications for it at home but is not on them in the hospital, figure out why because we don’t want that patients BP to skyrocket or (2) or if they are on thyroid meds at home but not inpatient, investigate why and if it should be also added, inpatient. (As a disclaimer, as you know they could be off of their home hypertension or thyroid meds for various reasons, so investigate!)], does the patient need the antibiotic that they are on (and if so, is it the right antibiotic)? is the vancomycin dosed correctly and is there an associated lab scheduled? If they are diabetic, are they on the proper insulin regime? Are meds that may require certain labs to be drawn (antiepileptics, certain antimicrobials…etc)? Point it, look at the patient profile, and focus on those kinds of interventions and then over time, as you learn other things, your interventions will become more expert-level.
- Keep open communication with your preceptor. If you need more time learning a concept, ask. If you have a question about something from rounds and you can’t find the answer, ask. If there is an urgent matter and you need help, ask.
- Next, HAVE GRACE WITH YOURSELF. You’re learning so many new things, getting used to different personalities, trying to do well, juggling all of the other resident responsibilities, and trying to maintain your life and sanity. It’s a lot. Trust me, I get it. Don’t feel pressured to have all the answers or to know it all. Everyone around you *should* know that you’re a learner and therefore you have room to grow and learn.
- Lastly, don’t compare yourself to others.
KEEPING TRACK OF ALL THAT YOU’RE DOING
During residency year (and as a pharmacist in general) documentation is soo important. It is especially important during residency because you are working towards something and that is getting a job and/or a PGY-2 afterward. When the time comes to go on your next journey of applying for your next step, it will come in handy to have documents about all the things you did and learned to refresh your memory and ace your next set of interviews.
So, with all that being said, please take it from me and log all interventions and activities that you did on that rotation – try to do this daily or at the end of every week. Also, note down any situations that you’d want to mention during an interview (remember those behavioral questions from residency interviews lol). This will also be helpful for the evaluations that you need to do throughout the residency year(s) as documentation that you’re learning/making a difference, for encouragement to see the progress you’ve made, and of course interviews/job apps.
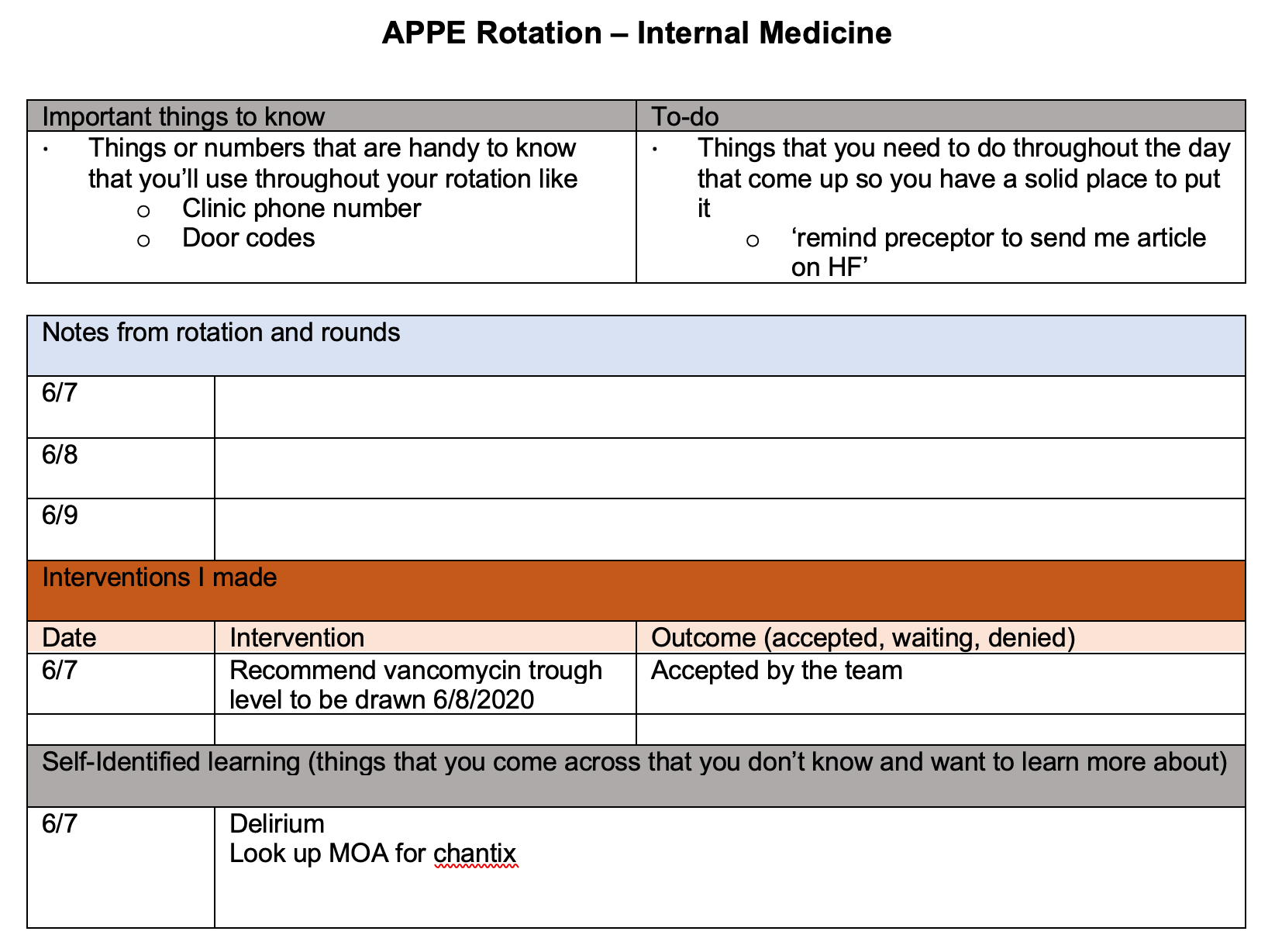
The above example is from my APPE rotation Tips Blog. I wanted to drop it here as an example of what you can include in your log. I would also suggest having a couple more sections at the bottom for any presentations & topic discussions you do while on that rotation (super helpful when revamping your resume) and another one with the links/citations/names for guidelines that are pertinent to that rotation.



click the images to go directly to the original posts!
STAYING EFFICIENT
There is always so much going on in residency that anytime you can figure out how to make your time more efficient, do so! You will come across various resources/protocols from the hospital, clinical guidelines (think diabetes, heart failure, IDSA guidelines), research papers/primary literature, cheat sheets, and drug conversions – just all kinds of knowledge in residency and it can be hard to keep up. Truth be told, you may not have time to read and learn everything (even though you may be working 60-80+ hours a week).
So, my biggest piece of advice is to create a document/system that you can access from anywhere (google docs, google drive, Microsoft Office 360..etc) and folders where you can save these for quick reference (make sure there’s no patient info). This will help you have a place to go when you need to reference a treatment algorithm or anything similar. I would also bookmark important hospital protocols and websites to get to them quicker as well. At my desk, I did have some algorithms/charts hanging up or in a folder if I found that I referenced them often so for example the ADA diabetes treatment algorithm, IDSA chart on treating pneumonia, Asthma/COPD graphic etc. This will help you have a quick reference to resources and answers throughout residency because you’ll find that you get asked the same questions again & again throughout the year even during your staffing shifts.
GENERAL TIPS THAT WILL HELP THROUGHOUT THE YEAR
- Reflect often! Throughout the residency year, you will get a lot of feedback, get asked to give feedback, and will need to give feedback about yourself. When you take the time to constructively analyze how you’re doing, what you’re doing well at (and how to continue/implement that throughout), and what you would like to improve (and HOW exactly you plan on improving) is very important and will help build your self-awareness.
- Don’t wait until you ‘know it all’ to jump in on a project. Residency is a year of learning. There will be times when you’re not sure how to tackle things. I recommend jumping in, doing the research, and taking initiative even if it makes you nervous at first (except when it involves patient care – in that case, ask for help when you don’t know and aren’t at the point of making critical decisions)
- Take advantage of being around so many experienced pharmacists. This will likely be one of the last times surrounded by great pharmacists which so much knowledge that you can learn from in the position of a learner.
- Take opportunities to learn seriously, don’t just go through the motions. When it comes time to perform at your job, you’ll be grateful you took the time to learn through that presentation you made (vs doing it rote) and that you paid attention during those (many) presentations and meetings. I know in residency it can feel overwhelming to learn through everything and sometimes some projects you just have to throw it together or multitask during meetings, so the point is, to choose wisely. In residency, it can be hard to give 100% to every single project/admin work you do – in fact, it was impossible for me and I think I had a pretty successful year despite that – I came to the realization that sometimes certain things just needed to get done vs. it being perfect 100% of the time.
- Be ready to teach yourself a lot of information and take charge of your own learning.
- Reflect and evaluate your career goals often to make sure you’re still in alignment to pursue them and to have honest moments with yourself if the specialty (if any) you’re pursuing is something you still want to do or if you want to switch it up.
- Here’s a typical list of things I know you already know but for completeness’ sake, here we go: be dependable, take ownership, understand your role as a pharmacist and ways to expand it, be on time, do good work, don’t gossip or be a chronic complainer, show eagerness to learn, be dependable, communicate openly, be an independent thinker, do good work consistently, always thinking of ways you can improve your project or even a process you see being done, speak up, prepare for meetings, and stay organized (again more on being organized to come in Part IV).
Lastly, residency is flat-out hard and chaotic most days. One of the biggest things I took away is that I’m able to handle a lot more than I thought. In the beginning, I didn’t know HOW I would complete all of the various tasks and responsibilities in residency + in my life but somehow I did. Your mind and capacity expand and you learn how to prioritize which will take you very far regardless of what your plans are post-residency. Remember this, it won’t last always! Thankfully residency is a defined period of time and many many people (including myself) have gotten through it! Looking back, I see the amazing benefits and opportunities that residency provided me and I wouldn’t change it.
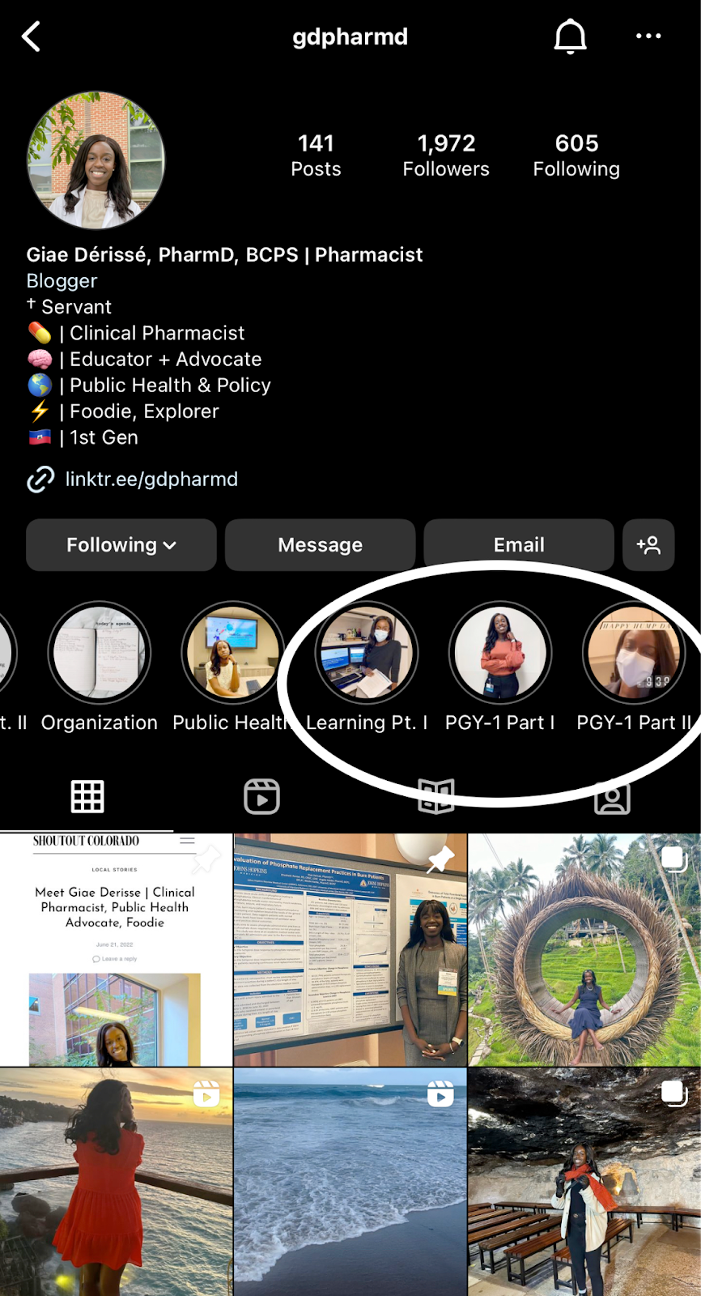
That’s all I have for now – I hope this was helpful! Definitely don’t hesitate to reach out to me via email or on Instagram if you have any questions and check out Part I about Residency prep & Part II about how to get the most out of orientation month. Stay tuned on Instagram to see when Part IV all about staying organized during residency comes out. If you want more about residency, check out my Residency Central Page. If you’re curious about what life was like for me when I was a pharmacy resident, Check out the highlights on my Instagram page (a screenshot with the specific highlights to look out for is to the right).
Work willingly at whatever you do, as though you were working for the Lord rather than for people. Remember that the Lord will give you an inheritance as your reward, and that the Master you are serving is Christ. Colossians 3:23-24 NLT
Practical Things I Used During Residency!
Top Pharmacy Apps You Should Try
Pass your Pharmacy Exams: BCPS and the MPJE
Getting Ready for Residency Part I: What to Do Before Starting
Getting Ready for Residency Part II: Orientation Month
Getting ready for Residency Part III: Rotation Tips as a Pharmacy Resident
Getting ready for Residency Part IV: Staying Organized during residency